Does Hormone Therapy Increase the Risk of Alzheimer’s?
It’s no surprise that many people are concerned about the conflicting headlines surrounding hormone therapy and its potential link to Alzheimer’s disease. But fear not, let’s dive into the real truth behind the data! The fine print is where you get the answers.
What is the REAL Truth?
When it comes to hormone therapy, the type of hormone used, and the timing are crucial factors. Some studies have shown increased Alzheimer’s risk, but here’s the catch – most of these studies were conducted on older women using synthetic hormones more than 10 years after menopause. It’s essential to distinguish between synthetic and natural hormones as they have different effects on the body.
Estrogen and the Brain
Estrogen, for instance, has neuroprotective properties that are vital for brain function. Estradiol is essential for brain function and up to 80% of peri-menopausal and post-menopausal women report neurological symptoms like hot flashes, mood swings, sleep issues, and cognitive changes.
Alzheimer’s disease affecting nearly twice as many women as men have shown associations. There is an association between menopause, Alzheimer’s and cognitive aging. 1
Only Bioidentical Progesterone Protects
The type of progesterone also matters. Natural, bioidentical progesterone has neuroprotective effects, whereas synthetic progestin does not. Sadly, these two are often lumped together in studies, leading to confusion in the findings.2
Estrogen and Progesterone Minimizes the Impact of Traumatic Brain Injury
Interestingly, both estrogen and progesterone have been found to minimize the impact of traumatic brain and spinal cord injuries. They offer protections through antioxidant effects, effects on brain cells, inflammatory response modulation, and cerebral blood flow and metabolism.3
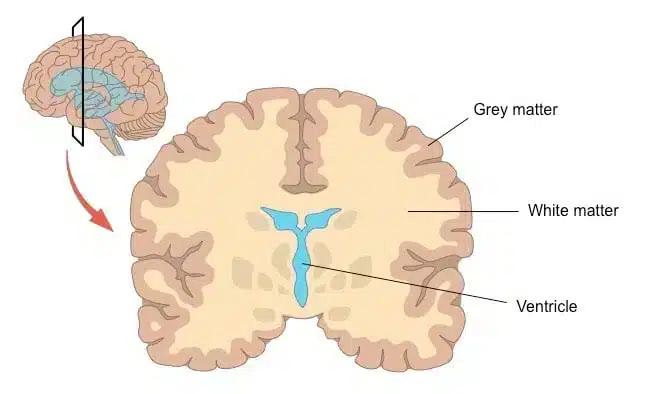
Memory, Learning and Brain Grey Matter Volume
In experimental models, rats without ovaries had impaired learning and memory, which was reversed when given estrogen.4 Menopausal women had lower brain grey matter volume in their brains in the regions that are vulnerable to developing Alzheimer’s disease. However, the longer a woman was exposed to hormones such as having a longer time beginning to the end of menopause, a higher number of children or hormone therapy, had more brain grey matter volume that correlated with better memory and cognition scores.5
Timing and Type are Important.
Timing is key in hormone therapy. Starting early and using natural bioidentical hormones for over a year has been associated with the greatest risk reduction for neurodegenerative diseases, including Alzheimer’s and dementia.
Hormone therapy with natural bioidentical hormones, with over a year duration of therapy was associated with the greatest reduced risk of all neurodegenerative diseases including Alzheimer’s and dementia. Neurodegenerative diseases included Parkinson’s disease (PD), dementia, multiple sclerosis (MS), and amyotrophic lateral sclerosis (ALS). The transdermal route of administration (estrogen through the skin) had the greatest risk reduction6
Multiple Risk Factors
Keep in mind that Alzheimer’s and neurodegenerative diseases have multiple risk factors. While hormone replacement therapy with natural bioidentical hormones can play a role, a personalized approach is essential. Addressing other risk factors like insulin resistance, chronic inflammation, low Vitamin D, hormonal deficiencies, and homocysteine levels is equally crucial.
Remember, it’s not just about treating one thing; a comprehensive evaluation of your risk factors and a tailored approach are key. If you’re interested in exploring bioidentical hormone replacement therapy and want to see if we’re a good fit, apply for a free clarity call. We’re here to guide and support you on your journey to optimal health and well-being.
Resources
- Jett S, Schelbaum E, Jang G, et al. Ovarian steroid hormones: A long overlooked but critical contributor to brain aging and Alzheimer’s disease. Front Aging Neurosci. 2022;14:948219. doi:10.3389/fnagi.2022.948219
- Singh M, Su C. Progesterone and Neuroprotection. Horm Behav. 2013;63(2):284-290. doi:10.1016/j.yhbeh.2012.06.003
- Brotfain E, Gruenbaum SE, Boyko M, Kutz R, Zlotnik A, Klein M. Neuroprotection by Estrogen and Progesterone in Traumatic Brain Injury and Spinal Cord Injury. Curr Neuropharmacol. 2016;14(6):641-653. doi:10.2174/1570159X14666160309123554
- ResearchGate, Engler-Chiurazzi EB, Singh M, Simpkins JW. Reprint of: From the 90׳s to now: A brief historical perspective on more than two decades of estrogen neuroprotection. Brain Res. 2016;1645:79-82. doi:10.1016/j.brainres.2016.06.016
- Schelbaum E, Loughlin L, Jett S, et al. Association of Reproductive History With Brain MRI Biomarkers of Dementia Risk in Midlife. Neurology. 2021;97(23):e2328-e2339. doi:10.1212/WNL.0000000000012941
- Kim YJ, Soto M, Branigan GL, Rodgers K, Brinton RD. Association between menopausal hormone therapy and risk of neurodegenerative diseases: Implications for precision hormone therapy. Alzheimers Dement (N Y). 2021;7(1):e12174. doi:10.1002/trc2.12174





She is a recognized and award-winning holistic, functional, integrative and anti-aging healthcare practitioner, speaker and author, and has been featured in ABC News, Forbes, WOR Radio and many media outlets to spread the word that you can live younger and healthier at any age.